Eating disorders can wreak destruction throughout a person’s life, much like substance use disorder can. When eating disorders and substance use disorder co-occur, the effects can be devastating unless treatment help is found.
In today’s age of staying fit and looking thin, it’s easy to see how an eating disorder can get started. Granted, not everyone falls prey to these types of societal pressures, those who do have plenty of cues to follow. As with most any chronic condition, eating disorders can take on lives of their own and place those affected at risk of developing other problems, like substance use disorder.
In fact, eating disorders and substance use disorder co-occur quite often and share similar symptoms that interact with each other. When left untreated, the effects of co-occurring eating disorders and addiction create a snowball effect that makes both conditions worse. The good news is, with the right treatment approach, you can break the hold these conditions have on your life.
What Are Eating Disorders?
Eating disorders, or ED for short, are behavior-based disorders that stem from destructive beliefs about food and body weight. People affected by eating disorders have a preoccupation with being thin so there’s a strong emotional component that drives eating behaviors. While anybody can develop harmful eating behaviors, women, aged 12 to 35, appear to be the most vulnerable.
The three most common types of eating disorders are:
- Bulimia nervosa – episodes of binge eating and purging
- Anorexia nervosa – restricting food intake and weight gain by limiting calories, using diet aids, using laxatives, vomiting, and engaging in excessive exercise
- Binge eating – eating large quantities of food in a short time on a frequent basis whether you’re hungry or not
In the case of bulimia nervosa and anorexia nervosa, feelings of low self-esteem and perfectionism fuel the extreme self-criticism that characterizes these conditions. Feelings of shame, guilt, and disgust about eating, in general, exist for all three types of ED. When left untreated, these conditions not only cause health problems but can also trigger other harmful behaviors, such as drug and alcohol abuse. For these reasons, the risk of developing co-occurring eating disorders and addiction increases considerably since feelings of guilt and shame can also develop from substance use disorder.
How Often Do Eating Disorders and Substance Use Disorder Co-Occur?
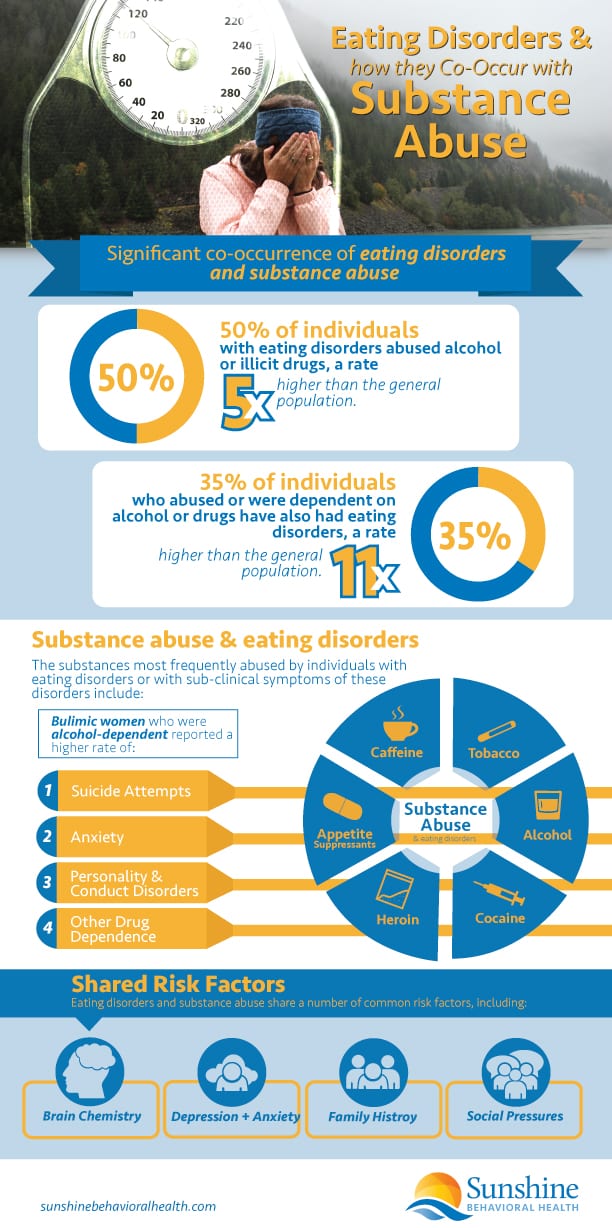
Co-occurring disorders don’t typically happen by coincidence but rather share certain characteristics that draw them together. A 2019 review of research on eating disorders and drug use shows 50 percent of people living with ED also struggled with alcohol or drug abuse. Compared to the general population, people ED sufferers are five times more likely to engage in substance use disorder. Among substance use disorderrs, as much as 35 percent also had eating disorders. This rate is 11 times greater than what occurs in the general population.
Stimulant drugs, such as cocaine and amphetamines are the most commonly abused for their slimming and euphoric effects, however, people with ED may abuse other substances for the same reasons, including: Heroin, Alcohol, Emetics, Caffeine, Nicotine, Diuretics, Diet pills, Insulin, and Thyroid medications.
Eating Disorders and Substance Use Disorder Resources
Whether you have an eating or substance use disorder or you suspect a loved one has a problem, there will no doubt be questions about everything from symptoms to dangers to treatment and support options. Below are some resources — both for educational and treatment purposes — to help you on your way.
Center for Discovery
The Center for Discovery offers counseling for teens and adults with eating disorders, mental health disorders, and substance use disorder issues. Online support groups (in-person ones are on hold due to COVID-19) are available for alumni, individuals in recovery, mental healthcare providers, and family and friends of anyone with an eating or substance use disorder. There is no cost to attend Center for Discovery support group meetings.
Eating Disorder Hope
Eating Disorder Hope offers treatment for eating disorders but also serves as a clearinghouse of information, specifically for online eating disorder support groups and organizations. Some meetings are tailored to specific eating disorders and led by an experienced therapist. (Those often have a charge per session.) Additional support group options are listed, similar to peer or 12-step patterns, with free meetings focused for various patients (women, adolescents, trauma survivors, etc.)
Multi-Service Eating Disorder Association (MEDA)
MEDA is a nonprofit with a mission to heal, inform, and empower through education, treatment, and referrals for individuals suffering from bulimia, anorexia, binge eating, and body image issues. MEDA also helps clients work through the underlying causes of their disorders and advocates for better acceptance of all body types.
Mayo Clinic
Eating disorders are complex, not simply a matter of consumption (or lack thereof), and fueled by numerous factors. The Mayo Clinic suggests a sort of roadmap to treatment. Step one: Visit one’s primary care practitioner or a mental health professional. From there a treatment plan can be modeled — one that includes medical and psychological therapies, nutrition education, medication (like antidepressants) for eating disorders, potential hospitalization or outpatient treatment, and an aftercare program.
National Center of Excellence for Eating Disorders
The National Center of Excellence for Eating Disorders (NCEED) was founded by the Substance Use Disorder and Mental Health Services Administration (SAMHSA). Its goals are two-pronged — to advance the education of healthcare providers and to raise public awareness of eating disorders and their treatment. The site has resources for individuals seeking help as well as for concerned loved ones and health professionals.
National Eating Disorders Association
The National Eating Disorders Association (NEDA) is a nonprofit that works to help individuals and families impacted by eating disorders. NEDA also continues to push for prevention, cures, and access to care. Site visitors will find screening tools, helplines, treatment options, support groups, studies, events, and information on co-occurring conditions.
Sunshine Behavioral Health
Eating disorders, like an addiction to drugs or alcohol, can take over a person’s life. The substance in question — it can be food, drug, or drink — takes top priority, harming one’s mental and physical health and upending their lives. Sunshine Behavioral Health focuses on substance use but understands the shared behavioral components that drive both drug/alcohol and eating disorders.
National Suicide Prevention Hotline
The National Suicide Prevention Hotline is a national network of crisis centers that offer support for people in emotional distress or who are contemplating suicide. Call 1-800-273-TALK (8255).
Similarities Between Eating Disorders and Substance Use Disorder
Behavioral Similarities
Anytime a behavior becomes a compulsion, addictive tendencies are at work. The need to engage in certain behaviors arises from ingrained patterns of thinking that are designed to satisfy an emotional need. These developments pave the way for addictions to take hold. Harmful eating behaviors and substance use disorder rest on behavior-based needs that satisfy underlying emotional distress.
The cravings aspect of drug abuse also applies with eating disorders. Like alcohol and drug abuse, someone with bulimia nervosa or a binge eating disorder will start to develop intense food cravings over time. Before long, cravings become so intense that you can no longer control how much you eat.
Binge eating can also produce mood-altering effects, much like alcohol and drugs do. In turn, overeating becomes a means to self-medicate feelings of depression or anxiety, which is what happens with alcohol and drug abuse. So, behavior-wise, eating disorders and substance use disorder tend to mirror one another.
Continuing to engage in destructive behavior in spite of the negative consequences is another key component of addiction. People struggling with ED often develop serious medical problems, such as dehydration, heart problems, cognitive impairments, blood sugar issues, and malnutrition. These conditions make it difficult to function effectively on the job or at school, and can also interfere with your ability to maintain healthy relationships. Like substance use disorder and addiction, the eating disorder becomes more important than everything else in a person’s life so negative consequences don’t matter.
Hereditary Factors
Both eating disorders and drug use run in families. While there may be environmental influences at work, genetic predispositions also exist. Molecular genetic research performed on twins and families show genetics account for 50 to 80 percent of the reason why a person develops an eating disorder. In fact, addictive genetic effects were found to be present for both conditions, which only reinforces the likelihood of someone developing co-occurring eating disorders and addiction.
Mental Health Issues
Both eating disorders and drugs interfere with the brain’s chemical activities. Since disorders, in general, are ongoing, their damaging effects on the brain’s chemical system continue for as long as the disorder continues. These effects create prime conditions for mental health problems to develop.
On the flip-side, mental health problems can actually make a person more susceptible to engaging in both eating disorders and drug use. Mental health problems commonly associated with eating disorders and substance use disorder include:
- Mood-based disorders, such as depression and bipolar disorder
- Anxiety-based disorders, such as generalized anxiety and panic attacks
- Post-traumatic stress disorder
When co-occurring eating disorders and addiction exist alongside a mental health disorder, the symptoms of one condition only works to intensify the symptoms of the other conditions, and vice versa. In effect, a vicious cycle of symptoms takes shape, making it that much harder to manage your life.
Shared Risk Factors
Not surprisingly, eating disorders and substance use disorder share certain common risk factors that increase your risk of developing both conditions. A 2003 study conducted by the National Center on Addiction and Substance Use Disorder set out to identify common characteristics and risk factors in people affected by substance use disorder and eating disorders. Here are a few similarities the study found between the two groups:
- Past sexual or physical abuse
- Destructive eating patterns and drug use tend to occur during times of stress or change
- Social peer pressures
- Dysfunctional childhood upbringing
- Susceptible to advertising messages
- A desire to emulate entertainment figures
As far as how individuals “fall into” harmful eating patterns and substance use disorder, both conditions tend to start out as experimentation. Then, experimenting soon turns into a way to protect or distract oneself from underlying emotional issues. As experimentation becomes more frequent, symptoms of both conditions start to take on a life of their own as cravings, withdrawal effects, and increasing tolerance levels drive eating and drug-using behaviors.
Their ability to take on lives of their own accounts for why eating disorders and addiction become chronic long-term conditions. Consequently, both conditions require comprehensive treatment approaches and both have high relapse rates.
Warning Signs of Co-Occurring Eating Disorders and Addiction
There are several red flags that a person may have an eating or substance use disorder, or a dual diagnosis of the two. Some signs may be obvious, like extreme weight loss (which may occur with either or both). Spotting other symptoms may take a bit more detective work.
Eating Disorder Signs
- Trying new diets and food fads, such as no carbs, no meat, or no dairy
- Highly critical of your body’s size, shape, and overall appearance
- Eating small amount of food at meal times, or skipping meals altogether
- Dental issues, such as tooth sensitivity, enamel erosion, cavities
- Noticeable weight gain or weight loss
- Dizziness, fainting
- Problems sleeping
- Muscle weakness
- Irregular menstrual periods
- Wounds take longer than normal to heal
- Your body feels cold most of the time
Signs of Addiction
- Loss of interest in activities you once enjoyed
- Spending more time other substance use disorderrs and less time with friends and family
- Noticeable declines in work or school performance
- Missed days at work or school
- Inability to focus or concentrate
- Obsession with getting and using drugs or alcohol
- Inability to control substance use disorder behaviors or stop using at will
- Abusing drugs or alcohol multiple times a day
- Money problems
- Problems with the law, such as DUIs
- A growing dissatisfaction with life in general
Signs of Co-Occurring Disorders
- Strong denial that a problem exists
- Fatigue, exhaustion
- Severe mental and emotional distress
- Suicide attempts
- Disorientation, confusion
- Job loss or expelled/suspended from school
- Driving loved ones out of your life
- Hospitalizations for medical emergencies and or psychological breakdowns
Treatment Considerations
While co-occurring eating disorders and addiction share many similarities, treating these two conditions requires different approaches. With substance use disorder, continued abstinence from drug and alcohol use is the sole objective. With eating disorders, an abstinence-based approach just isn’t practical since your body needs food to survive. Also, treating the two conditions separately can open the door for treatment gaps to work against your recovery efforts. For these reasons, it’s essential to receive treatment for both conditions at the same time.
A multidisciplinary treatment approach where symptoms of both conditions are treated simultaneously offers the best chance for a full recovery. To start, each person’s case is different so comprehensive screening and assessment should be done at the outset to determine your individual treatment needs. More often than not, drug or alcohol detox will require a structured treatment setting, so time in an inpatient or residential program will likely be necessary.
Depending on the severity of your condition, clinicians may use one or more therapeutic interventions, including:
- Medical treatment for any conditions that developed as a result of substance use disorder or harmful eating behaviors
- Education on how the two disorders play out in your daily life
- Behavior therapies
- Counseling
- Relapse prevention training
- Replacing destructive thinking surrounding food with a more balanced perspective on eating
- Developing healthy coping skills for managing cravings and destructive emotions
- Dietary education and planning
Since both conditions only get worse with time, it’s most important to seek out treatment help sooner rather than later. The longer eating disorders and drug use go untreated, the more ingrained these behaviors and their effects become. With proper treatment, patience, and a desire to get well, you can create a new and healthy lifestyle that sticks with you for the long-term.
Sources –
- Mayo Clinic, Eating Disorders
- American Psychiatric Association, What Are Eating Disorders?
- Neuropsychiatry, The Problem of Eating Disorders and Comorbid Psychostimulants Abuse: A Mini-Review
- Eating Disorders Catalogue, The Complex Relationship Between Eating Disorders and Substance Use Disorder Disorders
- Sunshine Behavioral Health, What Are the Traits Behind an Addictive Personality?
- Psychiatry, The Genetics of Eating Disorders
- National Eating Disorders Association, Anxiety, Depression, & Obsessive Compulsive Disorder
- Sunshine Behavioral Health, Co-Occurring Disorders
- The American Journal of Drug and Alcohol Abuse, Exploring the Relationship Between Eating Disorder Symptoms and Substance Use Severity in Women with Co-Morbid PTSD and Substance Use Disorders
- Social Work Today, Insatiable Hungers: Eating Disorders and Substance Use Disorder
- Sunshine Behavioral Health, Holistic Rehab Centers
- BMC Psychiatry, A Clinical Approach to the Assessment and Management of Co-Morbid Eating Disorders and Substance Use Disorders
- Center for Discovery, free eating disorder and mental health support groups
- Eating Disorder Hope, Online Eating Disorder Support Groups
- Eating Disorder Hope, Resources for Anorexia, Bulimia and Binge Eating Disorder
- Multi-Service Eating Disorder Association (MEDA) – MEDA’s Services
- Mayo Clinic, Eating Disorder Treatment: Know Your Options
- National Center of Excellence for Eating Disorders (NCEED), Our Mission
- National Eating Disorders Association (NEDA), Learn More About Eating Disorders
- National Eating Disorders Association (NEDA), Co-Occurring Conditions & Special Issues
- National Suicide Prevention Hotline, Call 1-800-273-TALK (8255)
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.






