The consequences of a traumatic brain injury (TBI) aren’t just physical but mental. People with a TBI are more susceptible to mental health issues, including substance use disorders, such as addiction.
A TBI is any injury that interferes with normal brain function. Typically, traumatic brain injuries are due to blows to the head, such as caused by a fall (almost half of all cases at 49%), vehicle crashes, bullet wounds, or being close to an explosion.
Most TBI cases are mild. They might escape notice, especially a closed head injury, with no break in the skull (open head). Any brain injury, however, can cause damage. That damage can be cumulative: the more brain injuries one has, the worse the overall effect.
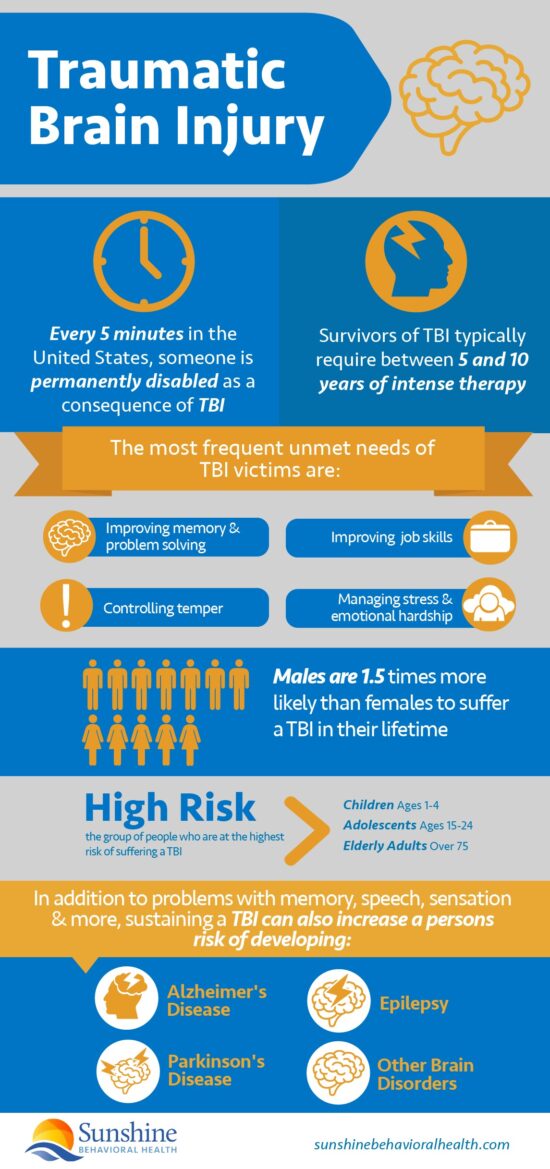
The aftermath of a traumatic brain injury is often life-changing for survivors, their families, and their caregivers.
Who Suffers from Traumatic Brain Injury?
TBIs are often associated with combat military personnel, as are similar and related conditions such as post-traumatic stress disorder (PTSD) and shell-shock. While PTSD often co-occurs with TBI, it is a distinct condition.
TBI is physical, such as injuries received due to an improvised explosive device (IED). PTSD is mental or psychological and may be caused by merely witnessing a traumatic event. In civilian life, watching an automobile accident could result in PTSD.
- A 2007 study estimated 10 million TBI cases globally, with 1.7 million United States emergency department visits annually. That didn’t include military TBI cases, suspected to be much more common.
- A 2012 study found that of the 2 million troops deployed to Iraq and Afghanistan since 2001, at least 23% or 220,000 reported at least one instance of TBI, though researchers suspect the actual number was higher.
- In 2016, the Traumatic Brain Injury Center of Excellence (formerly the Defense and Veterans Brain Injury Center) reported nearly 350,000 TBI diagnoses in the US military since 2000, involving somewhere between 10% and 20% of Afghanistan and Iraq veterans.
One problem with calculating the number of cases is that not all head injuries result in a TBI, not all TBIs are of equal severity, and TBI symptoms might not show up until weeks or months after the injury.
Symptoms of TBI
The Centers for Disease Control (CDC) estimate that about 2.8 million people per year seek emergency care for traumatic brain injuries. The CDC also estimates that as many as 5.3 million people in the United States are dealing with permanent effects of traumatic brain injury.
Even six months after a mild TBI, one in five individuals may start to experience severe physical, behavioral, cognitive, or mental symptoms, such as:
Physical
- Lack of muscle coordination.
- Speech problems.
- Weakness.
- Seizures.
Behavioral
- Loss of social skills.
- Lack of empathy.
- Self-centeredness.
- Emotional unavailability.
- Inability to control emotions.
- Mood swings.
- Triggers for anger and aggression.
- Constant frustration.
- Overwhelming depression.
Cognitive
- Short-term memory loss
- Lack of problem-solving skills
- Attention-deficit
- Loss of vocabulary, reading, and writing skills
- Poor judgment.
Mental
- Depression
- Anxiety
- Post-traumatic stress disorder (PTSD)
- Mood swings
- Difficulty concentrating
- Changes in sleep patterns (trouble getting to sleep or sleeping more than previously)
Treatments for TBI
Even with therapy, no treatment program addresses every challenge facing a survivor of traumatic brain injury. Recovery from a traumatic brain injury is an incremental process.
Some damage may be permanent or have unavoidable consequences later in life. The sooner it begins, the less damage.
Any treatment for TBI must address issues:
- Previous brain injuries. These may exacerbate the effects of a TBI. The more TBIs, the greater the odds of mental health disorders. If the TBI caused unconsciousness, the outcomes might be worse. Physicians and therapists may need to assemble a complete, detailed lifetime history of brain injuries, not just the most recent.
- An inhibited ability to learn. Brain injuries may make learning new therapies more difficult or impossible. Therapists may need to accommodate these deficits with sensory reinforcement (writing and watching) or make sure there are no distractions (noise, bright lights) during instruction.
- Holistic treatment. Many people with a TBI are on medications for behavioral problems or even substance use disorder, but TBI can affect how these medications affect them. If the individuals are undergoing several therapies at once, all must be considered and coordinated.
- Environmental influences. Understanding the social and physical factors that may make a health issue worse is even more necessary for the successful treatment of TBI than SUD. It also may take longer.
Relationship between TBI and SUDs
 One thing many people who experience TBI and SUD have in common is risk-taking behavior. Either or both could be caused by or the cause of co-occurring mental health issues.
One thing many people who experience TBI and SUD have in common is risk-taking behavior. Either or both could be caused by or the cause of co-occurring mental health issues.
There is evidence that substance use disorder rates usually go down after a TBI. At least, they do at first. Not that TBI is in any way beneficial. Possibly TBI inhibits one’s ability or desire to use drink or drugs.
As they recover or adjust (between two and five years), alcohol abuse may increase.
Between 10% and 20% may also start substance use disorder after a TBI, and they have worse overall outcomes than those who do not.
The main reasons people with TBI might start using and abusing alcohol, drugs, or other substances all boil down to coping with:
- Severe/chronic pain.
- Trauma.
- Depression.
- Aspects of their lives.
- Other underlying mental health issues.
More than 50% of people with TBI had alcohol in their systems at the time of the injury. Of that group, 20% required hospitalization, and 30% required rehabilitation.
Alcohol is so common before a TBI that all substance use may be ill-advised after a TBI. Some experts believe total abstinence after TBI is the only safe course, including alcohol and recreational drugs, whether legal or illegal.
TBI is also a stressor that may contribute to Alzheimer’s disease.
What is known is that TBI and substance use disorders often co-occur. Also, the best, evidence-based, most effective SUD treatments may not work as well for those with TBI without special considerations, such as:
- Longer and slower treatment. Individuals with TBI may be slower to comprehend than other people.
- More concise lessons. Use as few words as possible to explain a concept or treatment, but make them direct and concrete.
- Multisensory treatment. The effects of TBI affect the ability to learn but not intelligence. As with dyslexia, engaging as many of the five senses as possible may make the lessons stick better.
Treatment for SUDs
Most people who voluntarily enter treatment for substance use disorder will relapse. It’s not inevitable in any particular case, but that’s the statistical likelihood. Addiction hijacks the brain, changes its chemistry, and may not have a permanent cure.
One reason is that there is a genetic component to addiction. Some people are predisposed to SUDs. It doesn’t matter if they enter an addiction rehab center or attend 12-step meetings. Staying sober requires constant vigilance for some.
Treatments for SUDs include:
- Behavioral therapies. Based on psychotherapy (talk therapy), behavioral therapies teach people with SUDs to cope with their issues without using alcohol or drugs. These therapies include cognitive-behavioral therapy, motivational interviewing, contingency management, and family therapy.
- Medication-assisted treatment (MAT). Some drugs control opioid cravings and minimize withdrawal, such as methadone and buprenorphine (Suboxone). Others block opioids’ effects, such as naltrexone (Vivitrol).
- Peer fellowships. It may be simpler for some people to remain sober if they meet with other people who are doing the same. Alcoholics Anonymous and similar groups gather to share stories of their addiction struggles, their triumphs and failures.
Some, including AA, also use a process called the Twelve Steps to admit their problems, make amends to those they harmed, and commit to acting as mentors for others with the same difficulties.
Substance use may be more harmful to people with a TBI than a SUD alone, so it is even more vital that treatments address all of their circumstances:
- Do they want to stop using substances? A substance use disorder, such as addiction, is likely a lifelong condition, with relapse always a risk. It helps if they want to remain sober.
- Do they have co-occurring disorders? TBI is not the only condition experienced by people with SUDs. Anxiety, stress, trauma, and depression are also common. Treatment must be simultaneous and complementary.
- What type of therapy will they accept? MAT is one of the most effective treatments for opioid use disorder, but if the individuals don’t want to keep taking any drugs, this might be the wrong approach. Likewise, 12-step groups are a free, widely available, and promising means of getting people into therapy and remaining sober after formal rehab ends. They are often faith-based, however. That might not be a good fit for some people.
More study is needed on TBI and SUD to determine what is the safest way to recover.
TBI and Mental Health Resources
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.






