Mental health doesn’t happen in a vacuum; it also affects various parts of people’s lives and physical health, including their teeth.
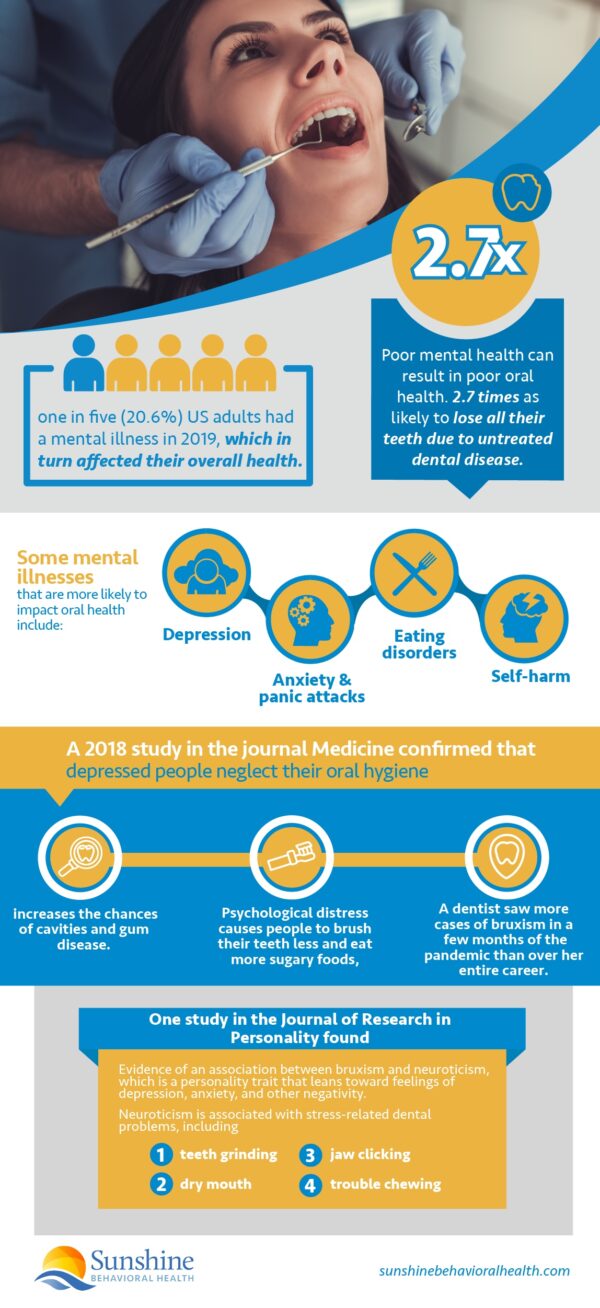
According to the National Alliance on Mental Illness (NAMI), one in five (20.6%) US adults had a mental illness in 2019, which in turn affected their overall health. People with mental health disorders have a higher risk of metabolic or cardiovascular diseases, substance use disorders, and poor oral health.
Dental symptoms can sometimes be signs of other health conditions. The American Dental Association says that gum disease can be connected to cardiovascular disease, stroke, and other metabolic health issues.
Poor mental health can result in poor oral health, too. Severe mental illness makes individuals 2.7 times as likely to lose all their teeth due to untreated dental disease.
Some mental illnesses that are more likely to impact oral health include:
- Depression
- Anxiety and panic attacks
- Obsessive-compulsive disorder
- Eating disorders
- Self-harm
- Psychosis
- Schizophrenia
There are steps people can take to improve both mental and oral health.
How Mental Health Impacts Oral Health
Mental health can cause oral health problems from numerous factors. These include:
- Neglecting oral hygiene and care.
- Other behaviors that impact dental health
- Side effects of medications.
Neglecting Oral Health
While depression comes with many symptoms, one that may impact dental health is feeling tired and unenergetic. With depression, even everyday tasks—such as proper oral hygiene—require a major effort. This could result in not brushing and flossing, or not putting enough energy into doing it properly. Other mental health disorders could have similar problems if a person’s state of mind is not focused on proper self-care.
A 2018 study in the journal Medicine confirmed that depressed people neglect their oral hygiene, both basic care and visits to the dentist. This increases the chances of cavities and gum disease.
Psychological distress causes people to brush their teeth less and eat more sugary foods, both of which impact oral health.
Behaviors that Harm Oral Health
In some cases, behaviors resulting from a mental disorder can impact the health of a person’s teeth and gums. The Oral Health foundation gives a few examples.
- One is that people with bipolar disorder or other similar disorders may brush their teeth too much and too aggressively, which is harmful because it can remove important enamel from the tooth’s surface.
- Those with anxiety may stay away from the dentist as a result of dental phobia. Avoiding the dentist or only having professional care rarely can increase the risk of dental issues.
- Another example given is dental erosion from people with the eating disorder bulimia. This results from the acid that reaches their mouth from vomiting their food. People with eating disorders can also have low calcium levels, which can be negative since calcium helps support the teeth.
Bruxism
Another problem is bruxism, which is the technical term for jaw clenching or teeth grinding. Numerous news articles across the internet have described dentists who have seen an uptick of bruxism during the coronavirus pandemic.
For example, in an article in The Washington Post, a dentist saw more bruxism cases during a few months of the pandemic than during the rest of her career.
The article notes that there is both daytime and sleep bruxism and that it’s common to move the jaws while sleeping. However, if the movements become forceful or too frequent, they can lead to dental symptoms such as jaw pain or tooth damage.
At the moment, the association of bruxism with the pandemic generally involves anecdotal accounts from dentists.
Nonetheless, in the September 2020 ADA Health Policy Institute’s COVID-19 impact poll, more than half of dentists saw a:
- 59.4% increase in the prevalence of bruxism in their offices.
- 53.4% increase of chipped or cracked teeth.
- 53.4% increase of symptoms of other temporomandibular (TMJ) disorders involving jaw pain.
Stress
More research is needed to prove a connection to the pandemic, but these are stress-related oral health conditions. The timing of the increase seems significant.
Previous studies have found an association between nighttime bruxism and mental health concerns such as stress, depression, or anxiety, although the results are often correlational.
Neuroticism
One such study in the Journal of Research in Personality found evidence of an association between bruxism and neuroticism, which is a personality trait that leans toward feelings of depression, anxiety, and other negativity.
The study found that neuroticism is associated with teeth grinding as well as other dental problems connected to stress, such as dry mouth, jaw clicking and having trouble chewing.
Earlier studies found anxiety and depression also often lead to bruxism.
Medication Side Effects
It’s not only the untreated symptoms of mental health disorders that can lead to oral health problems. Sometimes treatment creates new challenges. Medications people take for mental health disorders such as depression or anxiety are associated with the risk of oral health side effects.
According to the University of Washington School of Dentistry, some antidepressants that may have side effects of bruxism or xerostomia (dry mouth resulting from a lack of saliva flow) include:
- Selective serotonin reuptake inhibitor (SSRI) antidepressants.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs).
- Bupropion. An atypical antidepressant, bupropion may also cause gingivitis (gum disease) or glossitis (tongue inflammation).
- Tricyclic antidepressants (TCAs) are associated with potential side effects of dry mouth, salivary gland enlargement, or a discolored tongue.
Some benzodiazepines, which are often used for anxiety, have potential side effects of too much or too little salivation.
Dental Products and Treatments
A dentist may have advice on products and treatments that could counter some of these oral side effects.
- Xerostomia. The University of Washington School of Dentistry suggests artificial salivary products, fluoride toothpaste, fluoride gel, and xylitol gum, lozenges, or mints.
- Depression. RDH magazine says so-afflicted clients may benefit from a fluoride varnish treatment, dry mouth products, or an occlusal guard.
- Bruxism. The occlusal guard is helpful for anyone who grinds or clenches their teeth, regardless of whether they have bruxism or depression.
The Canadian Journal of Psychiatry article notes that mouthwashes or topical fluoride may be helpful.
Steps to Improve Mental Health and Oral Health
 A key role of professional dental care is to maintain good oral health and prevent dental problems from developing or worsening.
A key role of professional dental care is to maintain good oral health and prevent dental problems from developing or worsening.
Because mental health issues present challenges that may impact oral health, dentists take a full medical history from their clients, including mental health. Medications for mental health treatment may impact dental conditions or interact with dental drugs.
Regular Dental Appointments
Even when people don’t have a toothache or other obvious dental problem, regular visits are wise so the dentist can catch any problems before they become serious.
A small cavity is more easily drilled and filled than an abscessed tooth. If the clients are not caring for their teeth properly, that too can be corrected.
The same can apply to mental health problems. Some dental behavior such as grinding teeth may be related to a mental health issue. Dentists also may identify signs of depression and then offer support and referrals when needed.
Dental offices often set up the clients’ following appointments before they leave the office, making it easier to monitor, prevent, and treat future problems, dental and mental.
Seek Mental Health Support
Likewise, treatment for mental health difficulties or a disorder may also address an associated oral health concern.
A mental health provider—a counselor, psychiatrist, psychologist, or facility—makes a diagnosis and designs a treatment plan that may include therapy or medication, sometimes a combination of the two. Treatment varies due to the type of mental disorder, its severity, and whether there are any co-occurring conditions.
Because people with mental health issues don’t always take care of their health, including oral, mental health practitioners also may refer clients to dental providers when necessary.
There are checklists for non-dental professionals (the Canadian Journal of Psychiatry notes one) to assess the oral health of patients with mental health disorders. Mental health professionals can then help their clients find the appropriate dental practitioners as well as help with any anxiety about going to the dentist.
Be Mindful of Oral Health
When people are dealing with stress or other mental health disorders, including substance use disorder, they may not be mindful of their physical health, including dental.
Regularly scheduled appointments can help, as well as proper dental hygiene practices, but it may take the support and assistance of loved ones and professionals to ensure that they do. NAMI is an organization that provides education, support, advocacy, and other resources on mental illness. Its website offers information on mental health as well as resources such as online discussion groups and support groups. Also, the NAMI helpline is available to call for mental health support. Oral Health Foundation. This foundation offers support related to oral health. Its website provides information on oral and dental health, and the foundation carries out campaigns and activities to support these health areas. The Centers for Disease Control and Prevention (CDC) is the official health protection agency for the United States. The CDC offers a number of resources, including links to the National Healthy Sleep Awareness Project, American Sleep Association, American Sleep Apnea Association, Circadian Sleep Disorders Network, American Academy of Sleep Medicine, and the Sleep Research Society. This international non-profit organization helps people with anxiety and depression find the help they need. The Anxiety and Depression Association of America offers a wide variety of resources, such as: The Substance Use Disorder and Mental Health Services Administration (SAMHSA) offers a confidential 24-hour helpline — 800a662aHELP — for anyone experiencing symptoms of anxiety, depression, or other mental health issues. Trained representatives can provide information on locating local drug rehabilitation facilities, support groups, and community organizations offering mental health support.
Resources for Mental Health and Oral Health
National Alliance on Mental Illness (NAMI).
Centers for Disease Control and Prevention
Anxiety and Depression Association of America
SAMHSA National Hotline
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.






