Understanding suicide
Feeling hopeless, some people turn to drugs and alcohol as coping mechanisms. Others feel that nothing can help them. They think about suicide, make plans to kill themselves, and take their own lives.
The scenarios are common and connected and could function as a cycle.
People might be depressed, use alcohol, become even more depressed, drink more, and become so depressed that they begin to form suicidal ideas (display signs of suicidal ideation) and make plans to kill themselves, often while continuing to drink. Suicide might follow.
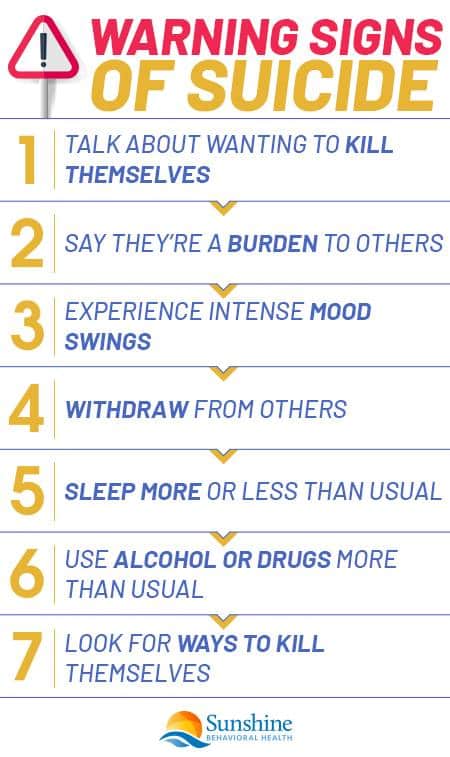
Warning signs of suicide
Certain signs might indicate that people are thinking about killing themselves. They could be serious about suicide if they:
- Talk about wanting to kill themselves or wanting to die.
- Say they’re a burden to others or they feel hopeless or in pain.
- Experience intense mood swings.
- Appear angry, irritable, anxious or discuss revenge.
- Withdraw from others.
- Sleep more or less than usual.
- Use alcohol or drugs more than usual.
- Research for ways to kill themselves.
Some people might not exhibit any signs, while others might display more than one. If people notice such signs in themselves or others, they should seek immediate assistance.
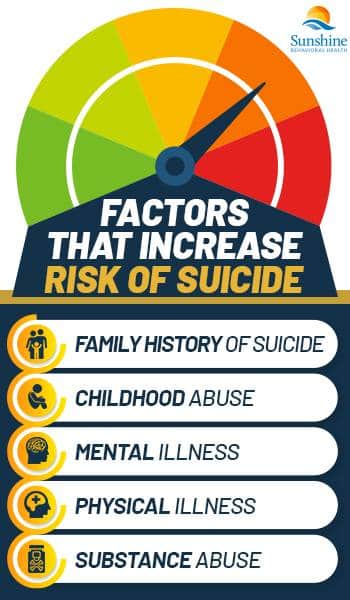
Factors that increase the risk of suicide
In addition to suicide warning signs, there are certain factors that might elevate a person’s likelihood to kill themselves. They include:
A family history of suicide or child maltreatment
Family histories of suicide could increase the odds of suicide. One study examined 243 people who had suicides in their families and found that:
- A little less than half (118) tried to kill themselves.
- More than half (137) had some sort of depression.
- A little more than a third (84) had mood disorders that periodically recurred.
Other familial and social factors may influence suicide. Childhood maltreatment occurs when people under the age of 18 experience neglect or physical, sexual, and/or emotional abuse. Researchers who examined several studies found that:
- Childhood emotional abuse doubled the likelihood of suicide attempts.
- Childhood physical abuse also doubled the chances that people would try to kill themselves.
- Childhood sexual abuse survivors were 3.5 times more likely to attempt suicide.
Such attempts may be common, as researchers estimated that 12.5% of U.S. children experience some form of child maltreatment.
Previous suicide attempt(s)
Past suicide attempts are another indicator of future suicide attempts.
A study of 1,490 people who received medical attention for suicide attempts found that 81 later killed themselves. In this group of 81 people, 48 of the people died after the attempt and 27 of the remaining 33 people died by suicide within a year.
Mental illness, particularly depression
Mood disorders and suicide often have close connections. According to some estimates, around 60% of people who kill themselves also have a mood disorder such as bipolar disorder, major depression, or dysthymia (longer-lasting mild depression).
Other mental illnesses are linked to suicide. Of the people who had attempted suicide in one survey, more than 70% had some sort of anxiety disorder. The likelihood of suicide was stronger for people who had both personality disorders that led to unhealthy ways of acting and thinking as well as a panic disorder or post-traumatic disorder (PTSD).
Physical illnesses and pain
Sometimes, people kill themselves because they can’t bear the pain and other symptoms of their physical illnesses.
Pain is also connected with other factors that can cause self-harming behaviors. For example, physical pain can cause or worsen depression leading to suicidal thoughts and eventually suicide. Or people might use drugs and alcohol to cope with pain but become addicted to such substances. Those addictions can make it more likely for one to commit suicide.
Hopelessness, impulsiveness, and aggression
 Depression and other mental illnesses can contribute to hopelessness, impulsiveness, and aggression. If people are depressed, they might lose hope. They might engage in impulsive or aggressive behavior because they feel that their lives aren’t worth living and they don’t fear the consequences.
Depression and other mental illnesses can contribute to hopelessness, impulsiveness, and aggression. If people are depressed, they might lose hope. They might engage in impulsive or aggressive behavior because they feel that their lives aren’t worth living and they don’t fear the consequences.
In one study of people hospitalized for suicidal thoughts, 91% of the people who later killed themselves scored a 10 or higher on the Beck Hopelessness Scale. This scale consists of 20 statements that respondents mark as true or false. It explores how people feel about expectations, motivation losses, and the future, and can help determine how hopeful people are.
Isolation
Isolation might contribute to hopelessness and suicide. Because of the COVID-19 pandemic, people have been encouraged to stay home or have been reluctant to go out.
Staying home may reduce the risks of catching a contagious virus, but it may also increase feelings of loneliness and isolation and eventually lead to suicide. Distress due to isolation and other aspects of COVID-19 have contributed to the suicides of many people since the beginning of 2020.
Epidemics of suicide
COVID-19 deaths are reminders that suicide isn’t an isolated incident. Aside from pandemic-related suicides, members of other groups have been taking their lives in large numbers.
One of these groups is females. According to the Centers for Disease Control and Prevention (CDC) and its National Center for Health Statistics:
- U.S. girls from the ages of 10 to 14 had a suicide rate that was more than three times higher in 2017 (1.7 deaths per 100,000 people) than it was in 1999 (0.5 deaths).
- The suicide rate for U.S. women aged 45 to 64 was 9.7 deaths per 100,000 people in 2017 and 6.0 deaths in 1999.
U.S. women who were 75 and older were the only group to see declines in the suicide rate from 1999 to 2017, indicating the growing problem of suicide in many groups.
Barriers to accessing mental health treatment
Despite the COVID-19 pandemic’s negative effects on mental health, many people have had trouble accessing adequate mental health treatment. These barriers can mean the difference between life and death.
Some traditional barriers to mental health treatment include:
- Fears that asking about suicide will trigger it.
- Inability to assess suicidal thoughts or behaviors.
- Lack of coordination among mental health assistance and other resources.
- Cost of treatment.
- Transportation problems.
- Stigmas surrounding mental health and seeking treatment for it.
- Discrimination surrounding people with mental health conditions, minority groups, and other populations.
When they have suicidal thoughts and behaviors, people are struggling. If they find it difficult to access care, they might not receive it.
Loss (relational, social, work, or financial)
Loss can also lead to suicide and other negative outcomes. Divorce is a type of loss. Different studies indicate that:
- Children raised by single parents have more than double the chances of becoming addicted to alcohol, developing a serious psychiatric condition, attempting suicide, or killing themselves.
- Divorced and separated men are more likely to commit suicide compared to married men.
Unemployment and financial worries are also losses that may drive suicide. Financial stressors may include:
- Lower earnings.
- Past homelessness.
- Unemployment.
- Financial problems such as debt.
Scholars have noted that if people experienced all four of these stressors, they were 20 times more likely to kill themselves than people who didn’t experience any of them.
Easy access to lethal methods
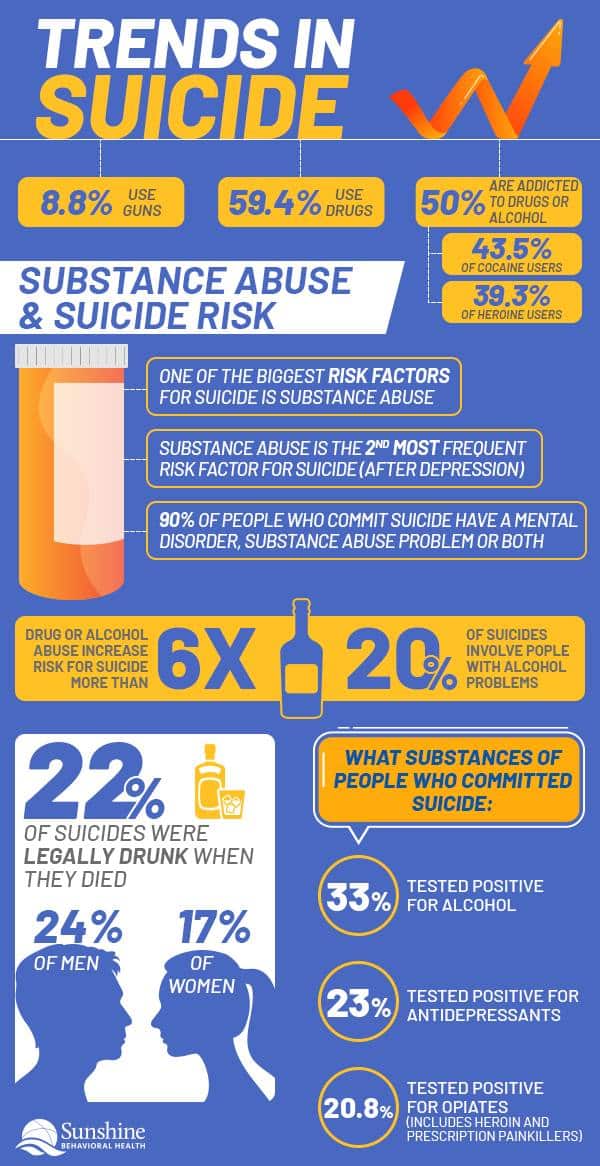
Easier access to lethal methods could increase the odds of people taking their own lives. Studies of U.S. suicide attempts from 2007 to 2014 indicate that:
- People used guns 8.8% of the time for suicide attempts. These events resulted in 75.3% of all deaths by suicide.
- People used drugs in 59.4% of all suicide attempts. These incidents accounted for 13.5% of suicide deaths.
While people use guns less often in suicide attempts, when they do, the results are more likely to be deadly.
Unwillingness to seek help due to stigmas
Compassionate mental health assistance can prevent people from killing themselves and other adverse outcomes.
But often, people don’t seek this assistance. They might worry that others will make fun of them, judge them, or deny them employment or other things if they admit that they’re thinking of suicide or have attempted it. They may also worry that others will stigmatize them for seeking help.
Stigmatization can lead to isolation, hopelessness, and other negative feelings. Negative feelings can make it more likely that people think about killing themselves or actually take such actions and less likely that they’ll seek assistance to deal with these thoughts and actions.
Alcohol or other drug misuse
 Alcohol and some drugs are depressants. That means they slow processes in the body. If people are already depressed and use depressants such as alcohol, they can become so despondent that they try to kill themselves, think about suicide, or make suicide plans.
Alcohol and some drugs are depressants. That means they slow processes in the body. If people are already depressed and use depressants such as alcohol, they can become so despondent that they try to kill themselves, think about suicide, or make suicide plans.
How prevalent is substance misuse and suicide?
The combination of suicide and substance use disorder is common:
- At least 25% of all people who misuse alcohol or drugs kill themselves.
- More than 50% of all suicides are related to a dependence on drugs or alcohol.
- Researchers believe more than 70% of all adolescent suicides might be related to alcohol or drug dependence and use.
Drugs and alcohol increase the odds that people will hurt themselves.
How addiction increases the risk of suicide
Physical effects from alcohol and drugs can make people feel more depressed, isolated, and suicidal. So can the psychological effects of substance use disorder and addiction.
Addiction can control many aspects of people’s lives. Satisfying their cravings for alcohol or drugs may become their main focus.
But being drunk or high is temporary. When the effects of alcohol or drugs fade, people might be depressed, feel ashamed of themselves, and worry about their addictions.
With those concerns, people might use more alcohol or drugs as coping mechanisms. But once the effects fade, their concerns might increase or even intensify, prompting additional substance misuse and addiction. This cycle is common, as about 30% of teenagers who have depression also have a problem with abusing drugs or alcohol.
Specific addictions and suicide
Substance use disorder, addictions, and suicides might be linked because:
- Common factors (family histories, abuse, pre-existing conditions) may contribute to substance use disorder and suicidal behaviors.
- Depression and other illnesses may drive substance use disorder and suicides.
- Being drunk or high could lead to risky behaviors that could prompt suicidal actions.
Certain substances may be tied to suicide and other negative outcomes.
Alcohol and suicide
The connections between alcohol and suicide are strong:
- Suicide is 60 to 120 times more common among people with alcohol addictions.
- People with alcohol addictions are 20 – 40% of all suicides.
Cocaine and suicide
Interviews of people who have used cocaine found that 43.5% had tried to kill themselves. It found that people who used cocaine and tried to kill themselves often were:
- Female.
- Younger.
- Prone to aggression.
- From families with histories of suicide.
- Dealing with childhood emotional neglect or physical abuse.
- Dependent on alcohol.
- Treated with antidepressants.
Heroin and suicide
Attempting suicide is also common in people who abuse heroin. A study found that 39.3% of people who abused heroin tried to kill themselves.
Characteristics of people who used heroin and tried to kill themselves were similar to people who used cocaine and attempted suicide. People who used heroin and attempted suicide tended to be:
- Younger.
- Female.
- Aggressive.
- Dependent on cocaine and alcohol.
- From families with histories of suicidal behavior.
Cannabis and suicide
Cannabis (marijuana) use and the presence of coexisting disorders can prompt thoughts of suicide. Among women who have had major depressive episodes and cannabis use disorders, 23.7% had developed suicide plans in the previous year, while 15.6% men who met the same criteria had such plans.
Studies of the National Surveys on Drug Use and Health determined that:
- 9.9% of men with cannabis use disorders but didn’t have major depressive episodes had suicidal thoughts.
- 3.0% of men who didn’t have cannabis use disorders or major depressive episodes had suicidal thoughts.
- 13.9% of women with cannabis use disorders but didn’t have major depressive episodes had thoughts of suicide.
- 3.5% of women who didn’t have cannabis use disorders or major depressive episodes had thoughts of suicide.
Warning signs of substance use disorder and suicidal thoughts
Signs of substance use disorder can be similar to signs of suicidal thoughts because both involve:
- Thoughts that can overwhelm people and interfere with their daily functioning.
- Neglecting ordinary activities.
- Isolating from loved ones.
- Engaging in dangerous and uncharacteristic behavior, such as lying, stealing, or having unprotected sex.
- Experiences changes in mood and activities.
- Talking about drugs, alcohol, suicide, feeling depressed, and other changes.
Recognizing such signs can help people address problems before they worsen.
How to help someone avoid suicide
 Talking about suicide could prevent it. Although people might be scared that talking about it will prompt people to kill themselves, talking won’t trigger suicides. Instead, people might be glad that others care about them and are willing to discuss matters with them.
Talking about suicide could prevent it. Although people might be scared that talking about it will prompt people to kill themselves, talking won’t trigger suicides. Instead, people might be glad that others care about them and are willing to discuss matters with them.
Loved ones can open the conversation with statements such as, “I’ve noticed that you’ve been going through some changes and was wondering if you wanted to talk about them” and “I’ve been concerned about you lately.” Then, they can ask questions directly:
- Are you thinking about killing yourself?
- Did you make any suicide plans?
- Have you tried to take your own life?
Such language doesn’t leave room for ambiguity and makes it more difficult to deny any problems.
Once people ask such questions, they should listen to the answers. Although the answers may be emotionally difficult, offering to listen without interrupting or judging can help people feel more comfortable to share potentially painful information.
When talking, people shouldn’t promise to keep things secret. They may need to reach out for further help. Instead, listeners should stay with the people sharing their stories and follow up afterward.
Listeners could remind people that even though they might not fully understand what’s happening, they support them and can help them find additional assistance.
Finding Help
Negative thinking can contribute to suicide and other outcomes. To end negative thinking, people might want to consider:
- Noticing negative thoughts as they occur.
- Using positive self-talk instead of more negative words and phrases.
- Engaging in uplifting activities instead of using negative talk.
- Paying attention to the positive aspects of their lives.
While negative thoughts can become habits and patterns, so can positive thoughts.
Therapists and support groups can help people embrace positivity and reject negativity. Using cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) can help people recognize negative thoughts and feelings surrounding suicide and help them develop more constructive thoughts, feelings, and actions.
Inpatient (residential) and outpatient programs can also help people with suicidal thoughts and behaviors, addictions, and other conditions. Resources can also help people if they’re struggling with suicidal thoughts. If people or their loved ones are having suicidal thoughts, they can call 911 or contact:
Resources for Suicide Prevention and Drug Abuse
Emergency resources
Other suicide prevention resources
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.